Developing Compliant Coding Queries: A Best-Practice Guide
Developing Compliant Coding Queries: A Best-Practice Guide
Accurate clinical documentation is foundational to high-quality patient care, proper reimbursement, and trustworthy quality reporting. When documentation is unclear, incomplete, or conflicting, compliant coding queries serve as the essential communication tool between clinical documentation integrity (CDI) professionals and providers.
This guide summarizes best practices taken from nationally recognized CDI standards and the “Guidelines for Achieving a Compliant Query Practice,” jointly developed by AHIMA and ACDIS, as presented in our quarterly webinar series.
What Is a Coding Query?
A coding query is a communication tool or process used to clarify documentation in the medical record to support accurate diagnosis and procedure code assignment. Queries support documentation integrity and ensure diagnoses are clinically supported and clearly stated in the record.
Effective queries must:
- Be compliant with the “Guidelines for Achieving a Compliant Query Practice”
- Be clear and concise
- Use applicable clinical indicators from the health record
- Include only clinically relevant response options
- Never reference financial or quality outcomes (e.g., reimbursement impact)
Ensure compliant, clinically supported documentation every time. Contact Sage Clinical RCM to enhance your CDI program with expert guidance and education.
Compliant Query Guidelines
To align with industry standards, compliant queries must adhere to these core principles:
- Present only health-record clinical indicators supporting the need for clarification
- Use optional answer choices such as unknown, other, inherent to, unable to determine
- Include clinically supported multiple-choice options only
- Avoid introducing unsupported diagnoses or implying financial motives
- Provide direct clinical citation when quoting the record
- Never mention reimbursement, quality scores, or reporting impacts
The AHIMA/ACDIS practice brief represents the industry standard for compliant queries.
Looking to strengthen query integrity and reduce compliance risk? Partner with Sage Clinical RCM for compliant CDI support and training.
When to Query
Queries are warranted when documentation requires clarification to ensure accuracy and clinical validity. Examples include:
- Supporting diagnoses that are clinically evident but not documented
- Resolving conflicting documentation
- Clarifying the reason for admission
- Confirming diagnoses referenced in pathology, radiology, or ancillary notes
- Establishing cause-and-effect relationships (e.g., complication vs. condition)
- Clarifying severity, acuity, specificity, or present-on-admission status
- Determining whether a history condition is active or historical
Ensure accurate diagnosis capture and reduce audit risk. Contact Sage Clinical RCM for CDI audits and provider education.
When Not to Query
A query should not be initiated when:
• No additional documentation supports a higher level of specificity
• Answer options cannot be supported by clinical indicators
• Documentation clarification is not clinically necessary
The query process should only be used to clarify – not create – clinical diagnoses.
Protect your organization from unnecessary queries and compliance exposure. Work with Sage Clinical RCM to implement best-practice query logic.
Types of Queries
There are three compliant query formats:
Open-Ended
Providers respond freely, allowing complete clinical explanation.
Multiple Choice
Includes only clinically supported options, plus an “other/unspecified” choice. Adding a new diagnosis option is allowed if supported by clinical evidence.
Yes/No
Used only for clarification of already documented diagnoses – not to introduce a new one.
Appropriate uses include: determining POA status, validating secondary diagnoses based on pathology, or resolving conflicting documentation.
Need help standardizing query templates? Sage Clinical RCM provides compliant query templates and CDI education.
The 3-Legged Stool Method for Constructing a Query
High-quality queries follow the 3-Legged Stool structure, ensuring compliance and clarity:
- Clinical Indicators
o Objective evidence from the record (labs, imaging, vitals, exam findings) - Risk Factors
o Relevant comorbidities, history, treatment course, or presenting symptoms - Treatment/Management
o Interventions supporting a diagnosis (medications, consults, monitoring, procedures)
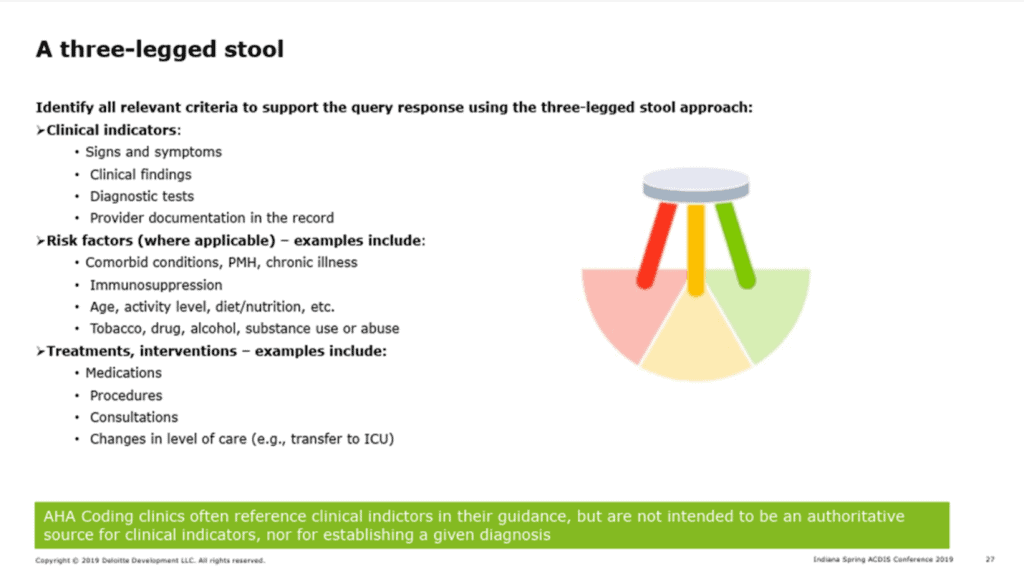
If one “leg” is missing, the query lacks the clinical foundation required for compliance.
Conclusion
Compliant queries ensure documentation integrity, support accurate coding, improve clinical communication, and reduce compliance risk. By adhering to AHIMA and ACDIS standards and using clinically driven methodology, organizations can achieve:
- Clearer clinical documentation
- Accurate code assignment
- Audit-ready records
- Trusted data and reporting
Ready to enhance CDI quality and compliance? Contact Sage Clinical RCM for CDI services, compliant query training, and provider education.