Stop the Downgrades: Proven Tactics to Defend Your DRG Coding Assignments
Stop the Downgrades: Proven Tactics to Defend Your DRG Coding Assignments
DRG downgrades are a costly threat to revenue integrity. According to the 2024 Experian State of Claims report, 77% of providers reported an increase in claims denials. Nearly half of the respondents (46%) cited missing or inaccurate information as the leading cause. Now more than ever, hospitals and health systems need to strengthen their DRG coding validation, documentation workflows, and appeal strategies to safeguard their reimbursements.
From documentation pitfalls to payer pushback, successfully navigating DRG coding challenges requires a deeper understanding of common triggers, the ability to proactively identify high-risk cases, and a data-backed approach to building bulletproof appeals. I’ve compiled best practices and other helpful insights to help your team stay ahead.
Recognizing the Most Common DRG Downgrade Triggers
Payers are increasingly scrutinizing certain high-value diagnoses, using clinical validation criteria that may differ from those applied by providers. These discrepancies often result in downgrades, and, if unaddressed, significant financial impact.
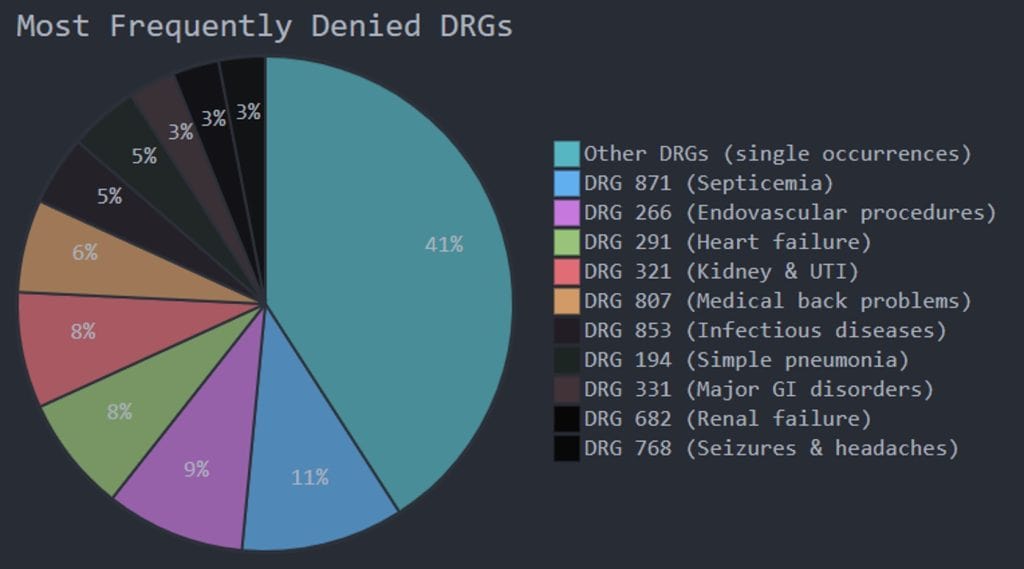
Let’s examine the most common diagnostic categories that raise red flags:
Sepsis
Still one of the most hotly contested diagnoses, sepsis is frequently challenged when documentation fails to align with Sepsis-3 clinical criteria, or if blood cultures return negative. Payers often argue: “Only meets SIRS criteria, not sepsis,” or cite inconsistent provider documentation.
Prevention Strategy: Ensure clear and consistent documentation across all notes, highlight a provider-documented source of infection, and cite specific clinical indicators like SOFA score, temperature, respiratory rate, or leukocytosis.
Respiratory Failure
Conflicting terminology (acute vs. chronic vs. acute-on-chronic) alongside weak ABG documentation or vague descriptions of oxygen needs often results in denials.
Prevention Strategy: Align documentation with ABG thresholds and include supporting evidence such as oxygen requirement beyond baseline, increased work of breathing, and intervention details.
Malnutrition and our Case Study on the consistent application of the ICD-10 code for severe protein-calorie malnutrition
Payers frequently reject malnutrition diagnoses due to insufficient support from dietitian assessments or missing indicators, like weight loss percentage or physical exam findings.
Prevention Strategy: Include BMI, lab values, physical findings (e.g., temporal wasting), and a clear nutritional intervention plan.
We assisted one client in developing a standardized process for addressing severe protein-calorie malnutrition diagnoses by conducting comprehensive inpatient coding audits over a three-year period. Our dedicated consultants created and implemented a streamlined review form template that enabled inpatient coders to efficiently submit their documentation findings to the hospital’s Physician Advisor.
This case study not only highlighted the importance of coding compliance with the Office of Inspector General but also identified educational opportunities for ensuring the consistent application of the ICD-10 code for severe protein-calorie malnutrition, ultimately improving documentation standardization and medical coding quality assurance. Download our case study here.
Encephalopathy
Diagnosis is commonly denied when altered mental status is attributed to medication effects or when clinical indicators aren’t captured consistently across the record.
Prevention Strategy: Use mental status assessments (e.g., CAM, MMSE), document the temporal relationship to the underlying cause, and show provider concern beyond the discharge summary.
Spotting High-Risk Cases Before They Become Denials
Being proactive is key. Coders, auditors, and CDI teams must be trained to identify vulnerabilities early.
Here are three red flags that often signal a potential downgrade:
- Inconsistent Documentation: When one provider documents sepsis but another refers only to “fever” or “infection,” this inconsistency opens the door for clinical validation denials.
- Coding Vulnerabilities: If one MCC is solely responsible for the DRG shift, and that diagnosis lacks strong support, you’re at high risk.
- Short Length of Stay: Complex diagnoses paired with brief admissions (e.g., three-day stay for sepsis and encephalopathy) can prompt payer suspicion. Implementing “pre-bill clinical validation” reviews for high-risk diagnoses and short stays can make all the difference.
Building Strong Clinical Support for DRG Coding Assignments
Even when documentation seems sufficient, coders and CDI teams must ensure alignment with both coding and clinical validation guidelines.
Here are a few key steps to build strong support for DRG assignments:
- Map clinical indicators to each diagnosis: Identify and organize lab values, imaging findings, treatments administered, and provider observations.
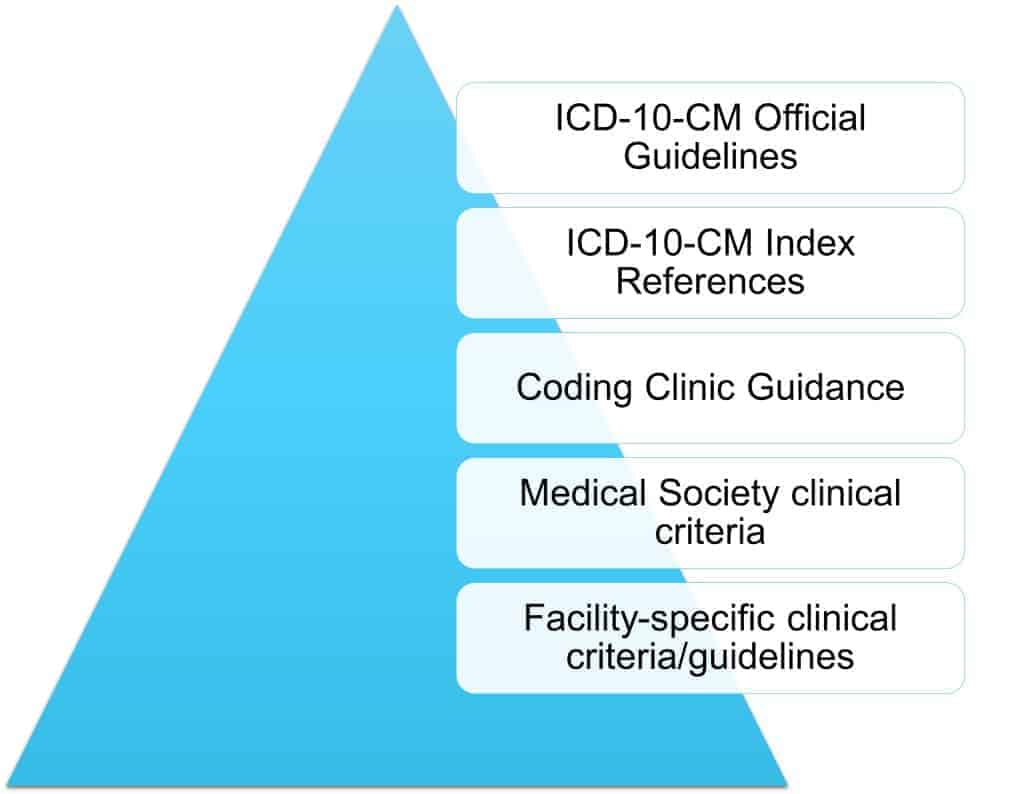
- Leverage guidelines and references: Include AHA Coding Clinic guidance, ICD-10-CM Official Guidelines, and clinical resources like CDC or Sepsis-3 definitions.
- Standardize provider queries: Create templates that prompt precise terminology for diagnoses frequently denied, such as respiratory failure, malnutrition, or sepsis.
- Conduct second-level coding validation before an appeal is ever needed: Don’t try to defend indefensible coding. Verify POA indicators, encoder logic, and adherence to official rules.
Mastering the DRG Appeal Process
When a DRG is denied, a well-structured and supported appeal can recover lost revenue. An effective appeal isn’t just a rebuttal. It’s a clinically detailed, guideline-supported argument that tells the patient’s story with clarity.
Essential Appeal Components:
- Clear Statement of Dispute: Identify the denied DRG, the proposed DRG, and the rationale given by the payer.
- Timeline of Clinical Events: Walk through the patient’s stay day by day. Use objective timestamps and reference labs or interventions.
- Mapped Clinical Evidence: Align every indicator (labs, vitals, imaging, treatment) with the diagnosis in question. Use reference ranges.
- Guideline Citations: Quote relevant Coding Clinic issues and official guidelines, as well as any facility-specific clinical criteria and guidelines.
- Direct Documentation References: Include excerpts from physician notes to reinforce the diagnosis.
- Conclusive Summary: Clearly state why the original DRG is appropriate and request reinstatement.
Case in Point:
A DRG 871 (Septicemia with MV >96 hrs) was downgraded to DRG 177 (Respiratory Infection). On appeal, the team outlined a clinical timeline from ED presentation to intubation, referenced Sepsis-3 and POA guidelines, provided blood culture results and ventilator logs, and quoted physician documentation confirming sepsis. The result? A successful DRG reversal.
Optimizing Your DRG Coding Defense Strategy
To reduce denials and increase appeal success, organizations should take a holistic, workflow-based approach:
Coding and CDI Team Actions:
- Assign a denial prevention specialist to review cases pre-bill
- Implement a 48-hour review process for cases with a single MCC
- Conduct pre-bill clinical validation for high-risk diagnoses
- Build a “citation library” of Coding Clinics for commonly denied diagnoses
Physician and Provider Engagement:
- Share denial trends with physicians to guide documentation habits
- Develop targeted provider education based on denial patterns
- Use physician advisors for complex clinical validation reviews
Organizational Improvements:
- Track appeal outcomes by coder, provider, and service line
- Measure financial impact of downgrades and set benchmark appeal success rates
- Build payer-specific appeal templates based on historical trends
Whether you’re dealing with sepsis, respiratory failure, malnutrition, or encephalopathy, YES can help you stay one step ahead with audit-ready support, customized education, and proven strategies to strengthen your coding and appeal outcomes. Reach out to our consultants today so we can help you turn those DRG downgrades into recovered revenue.


