HCC Coding Cheat Sheet 2023: Cracking the Code on the Most Commonly Missed & Confusing HCC Codes
HCC Coding Cheat Sheet 2023: Cracking the Code on the Most Commonly Missed & Confusing HCC Codes
Defining the CMS-HCC Model Overview
Before we discuss the commonly missed or confusing HCC codes of 2023, let’s review the mechanics of the CMS-HCC risk adjustment model. The CMS-HCC model is prospective where data is collected in the base year to determine expected costs for the following year (the “prediction” year). For example, data from 2022 (base year) will predict expenses in 2023 (prediction year).
Each segment of the CMS-HCC model relies on data from demographics (i.e. patient’s age and gender) and health status. These are based on ICD-10-CM diagnosis codes to predict costs.
To identify the disease diagnoses that predict future healthcare costs, HCC models first organize diseases/conditions into body systems or disease processes, called diagnostic groups (DXGs). The disease processes within each diagnostic group (DXG) fall into condition categories (CCs). Then, they are delineated into the HCC. For more information about this process, review our HCC Medicare Advantage Background and Overview article.
Currently, version 24 for the payment year 2023 includes 86 HCCs along with a set of 24 age-sex indicator variables. There is also a set of payment HCC count variables to better capture the higher costs of beneficiaries with multiple HCCs. Each HCC category equates to a specific value for a risk adjustment factor (RAF) score.
The Centers for Medicare and Medicaid Services (CMS) uses the CMS-HCC risk adjustment model for the Medicare Advantage program and those who qualify for Medicare or patients 65 and older, calculating risk payments for the next year. The RAF score is used to calculate expected future health costs for each patient. Instead of providing one base payment for every patient, the risk adjustment model allows for more accurate payments for expected costs based on every enrollee’s health status and demographics.
As HCC coding experts, we understand the importance of accurate HCC coding for healthcare providers and insurance companies. Accurate HCC coding is crucial because it allows for more accurate payments for expected costs based on every enrollee’s health status and demographics. With the CMS-HCC risk adjustment model calculating risk payments for the next year, it becomes essential to ensure that accurate codes are used to reflect the patient’s health status. This ensures that the healthcare provider receives the appropriate reimbursement for the care provided, while insurance companies can better manage their risk.
The HCC Code Maze
The HCC coding system is complex and ever-evolving. Therefore, it is essential to stay up-to-date with the latest changes and ensure that the correct codes are used to reflect the patient’s health status. These constant updates make it challenging for healthcare providers and insurance companies to ensure accurate reimbursement and appropriate risk management.
ICD-10-CM diagnosis coding for HCC reporting is different from traditional ICD-10-CM diagnosis coding because the intent is to report all conditions that affect the individual’s health status concurrently across the continuum of care.
To support an HCC, clinical documentation in the patient’s health record must support the presence of the condition and indicate the qualified provider’s assessment and/or plan for management of the condition. Validation of medical record eligibility includes patient identification in the record, ensuring the provider is an eligible provider, and verifying that the record has been authenticated.
The entire listing of 2023 HCC categories with applicable ICD-10-CM diagnosis codes can be downloaded here.
Here is a table of the most common chronic diagnosis conditions for HCCs currently listed by CMS:
Each applicable ICD-10-CM diagnosis code is assigned to a specific HCC, and each HCC has an associated RAF.
For CMS-HCC V24, RAF scores vary from 0.105 to 2.659. For a visual example, below is a listing of select HCCs with their associated RAF – Community RAF for aged, not disabled, not eligible for Medicaid (Non-Dual).
| HCC | Descriptor | RAF Score |
| HCC 1 | HIV/AIDS | 0.335 |
| HCC 2 | Septicemia, Sepsis, Systemic Inflammatory Response Syndrome/Shock | 0.352 |
| HCC 6 | Opportunistic infections | 0.424 |
| HCC 8 | Metastatic Cancer and Acute Leukemia | 2.659 |
| HCC 9 | Lung and Other Severe Cancers | 1.024 |
| HCC 10 | Lymphoma and Other Cancers | 0.675 |
| HCC 11 | Colorectal, Bladder, and Other Cancers | 0.307 |
| HCC 12 | Breast, Prostate, and Other Cancers and Tumors | 0.150 |
| HCC 17 | Diabetes with Acute Complications | 0.302 |
| HCC 18 | Diabetes with Chronic Complications | 0.302 |
| HCC 19 | Diabetes without Complication | 0.105 |
Our firm’s coding consultants are HCC experts who receive ongoing education and training on the latest updates and changes to the HCC codes. We understand that accurate HCC coding is critical for providers and insurance companies, and we strive to remain compliant with the latest updates. Our team of subject matter experts has years of experience in the field and uses their knowledge to provide accurate coding services that help providers and payers alike.
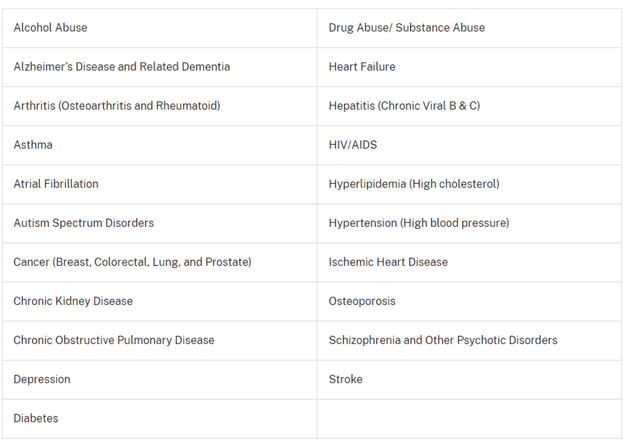
Deciphering the Top 5 Commonly Missed HCC Codes
Listed below are some of the most frequently missed ICD-10-CM diagnosis codes that equate to an HCC category:
- Artificial opening status – tracheostomy (Z93.0 HCC 82), gastrostomy (Z93.1 HCC 188), ileostomy (Z93.2 HCC 188), colostomy (Z93.3 HCC 188), cystostomy (Z93.50 HCC 188), urinary tract (Z93.6 HCC 188)
- Dependence on renal dialysis (Z99.2 HCC 134), Dependence on respirator (ventilator) status (Z99.11 HCC 82)
- Long term (current) use of insulin (Z79.4 HCC 19)
- Amputation Status Codes – Acquired absence toe(s), foot, ankle (Z89.411 – Z89.449 HCC 189)
- Functional quadriplegia – Complete immobility due to severe physical disability or frailty (R53.2 HCC 70)
In order to support an HCC, the medical record must include the presence of the disease/condition and the clinical provider’s monitoring, assessment, evaluation, and/or plan for management of the disease/condition.
The Confusing Conundrum: HCC Codes That Baffle
There are some HCC codes that are more perplexing than others, have a necessity for another ICD-10-CM diagnosis code connection, or need detailed specificity. Here are some examples:
- Body mass index (BMI) 40 or greater, adult (Z68.41-Z68.45 HCC 22): According to the Official Coding Guidelines for ICD-10-CM I.B.14, the BMI may be documented by other clinicians involved in the care of the patient (e.g. dietitian); however, the associated diagnosis (such as overweight, obesity, morbid obesity) must be documented by the provider. Many times, the BMI is listed, but there is no documentation of obesity or morbid obesity. Both diagnoses are essential for appropriate code and HCC assignments. For instance, if the patient’s BMI of 40.5 is documented, no code is assigned and, therefore, no HCC. However, if the diagnosis of morbid obesity (E66.01) is also documented, along with the BMI 40.5 (Z68.41), then both codes can be accurately assigned resulting in an HCC 22 (morbid obesity), an additional relative risk factor of 0.250.
- COMA Scale (R40.2110 – R40.2444 HCC 80): According to the Official Coding Guidelines for ICD-10-CM I.C.18.e, the coma scale codes (R40.21- to R40.24-) can be used in conjunction with traumatic brain injury codes. They are primarily used by trauma registries, but they may be used in any setting where this information is collected. The Coma Scale codes should be sequenced after the diagnosis code(s). Like the BMI documentation, the Coma Scale may be documented by other clinicians, but the associated diagnosis (traumatic brain injury) must be documented by the provider. Some, but not all, of the Coma Scale codes equate to HCC 80.
- Diabetes HCCs 17, 18, 19: Diagnosis specificity documented by the provider is essential for correct HCC code assignments. One of the most common diagnoses documented is “Diabetes,” which is assigned to code E11.9 (Type2 diabetes without complications) and equates to HCC 19 with a RAF score of 0.105. In comparison, if the provider documents Type 2 diabetes mellitus with hyperosmolarity (E11.00-E11.01) or Type 2 diabetes mellitus with ketoacidosis (E11.10-E11.11), both of which equates to HCC 17 RAF score 0.302. In contrast, if the documentation by the provider states Type 2 diabetes mellitus with diabetic nephropathy E11.21 or Type 2 diabetes mellitus with diabetic cataract E11.36, both of which equate to HCC 18 RAF score 0.302.
- History of Cerebral Infarction vs Cerebral Infarction with residual deficits: The documentation details surrounding a “history of stroke” is essential in correct code assignments. ICD-10-CM diagnosis code Z86.73 describes Personal history of transient ischemic attack (TIA), and cerebral infarction without residual deficits, which is an important code assignment for capturing the patient’s clinical history. However, it does not lead to an HCC. But, if the provider documents that the patient does have some residual deficits from a stroke, then an ICD-10-CM diagnosis code from category I69, Sequela of cerebrovascular disease, can be assigned and could be assigned to an HCC. For example, ICD-10-CM diagnosis code I69.051 (Hemiplegia and hemiparesis following nontraumatic subarachnoid hemorrhage affecting right dominant side) equates to HCC 103 RAF score 0.437.
- Chronic Kidney Disease (CKD): As previously stated, documentation specificity is key to correct code and HCC assignment. And for CKD, the documentation of the CKD stage is essential. For example, CKD Stage 4 (N18.4 HCC 137 RAF 0.289) versus CKD unspecified (N18.9 no HCC). Also, many times, CKD is associated with hypertension or diabetes which is guided by the Official Coding Guidelines for ICD-10-CM regarding additional ICD-10-CM codes as well as sequencing. For comparison, CKD Stage 5 due to Type 2 diabetes mellitus with diabetic chronic kidney disease would result in the following code assignments: (E11.22 HCC18 RAF 0.302) and (N18.5 HCC 136 RAF 0.289).
HCC Coding Cheat Sheet 2023: Tips and Tricks for Success
Regular monitoring for correct coding is considered a best practice for both healthcare provider organizations and payers due to the complexity of documentation and coding required for accurate HCC capture. Risk adjustment coding leaders should keep a close eye on the following common coding errors:
- Reporting only the primary or principal diagnosis
- Coding rule-out, possible, or probable diagnosis codes from outpatient records
- Coding resolved or historical conditions as current (e.g., MI or CVA)
CMS has established a formal audit program to monitor health plan compliance with HCC reporting regulations. The program includes Risk Adjustment Data Validation (RADV) audits, which are intended to ensure that health plans receive the appropriate risk adjustment based on the health status of their patients. As a result, accurate and complete documentation and coding are critical for the identification of HCCs.
Annual HCC re-training for both providers and coders is essential. Note that many Medical Schools are now training their physicians on the importance of documentation and HCC specificities and coding accuracy.
YES specializes in providing HCC education to healthcare providers and corporate coding teams. We understand the complexities involved in accurate HCC coding and can provide comprehensive training to ensure that your team is well-versed in the latest changes and regulations. With our expert guidance, you can rest assured that your organization is accurately capturing patient risk and receiving appropriate reimbursement for your services.
If you’re searching for top-notch HCC coding support services, our firm can provide this type of assistance. We ensure accurate reimbursement and appropriate risk management for our clients, leading to better healthcare outcomes and more efficient utilization of resources. Partner with us and take advantage of our expertise to achieve optimal results.
YES Can Be Your Trusted HCC Coding Partner
In conclusion, HCC codes play a significant role in the healthcare industry, impacting everything from patient care to reimbursement rates. However, some codes are commonly missed or confusing, so it’s important to stay updated and master HCC coding. By doing so, healthcare professionals can help ensure accurate and fair reimbursement, as well as better patient outcomes.
YES’ coding support services are a great resource to turn to. Let’s work together towards a brighter future for healthcare.
Additional HCC Coding Resources:
- Upcoming Changes to 2024 CMS-HCC Risk Adjustment Model
- Maximizing Reimbursements Through Effective HCC Coding Companies
- HCC Coding 101: How to Avoid Scrutiny as Risk Adjustment Schemes Come to Light
- HCC Consulting Case Study: Bridging the Gap Between Medical Software Companies & Coding
- How HCC Medical Coding Can Turn Your Healthcare Organization into a Profitable One
- Your Quick Guide to HCC Risk Adjustment Models
- HCC Coding Best Practices
- HCC Conditions and M.E.A.T. Criteria